As medical education evolves, the concept of competency-based training has gained significant traction in recent years. One of the key elements of this approach is the use of Entrustable Professional Activities (EPAs).
In this article, we will explore the role of EPAs in medical and healthcare education, their development and implementation, and the impact they have on shaping the future of healthcare professionals.
Understanding Competency-Based Medical Education
The shift in thinking from focusing on the essential knowledge of a profession to the purpose of education and what students can actually do in real-world clinical environments has paved the way for competency-based medical education. This approach emphasises the outcomes of training and aligning them with the needs of society. It focuses on progressive sequencing of competencies, considering how learners develop their understanding and skills from novice to expert. Time is viewed as a resource rather than a driver of educational programmes, with learning experiences structured to resemble the practice environment. Teaching is tailored to competencies, emphasising learning through experience and application. Finally, assessment is key, with regular low stake assessments to measure performance and ensure readiness for the field.
What do Entrustable Professional Activities (EPAs) Assess?
EPAs measure to what level a learner is trusted to perform a task and can be used in a range of settings and form a central component of competency-based medical and healthcare education. EPAs are not an alternative for competencies, but a means to translate competencies into clinical practice. They are specific activities or tasks that learners should be able to perform without direct supervision by the end of their programme. These EPAs cover a range of essential skills and responsibilities and might include tasks such as gathering a patient's history and performing physical examinations, recommending and interpreting diagnostic tests, documenting clinical encounters, collaborating as part of an interprofessional team, and identifying system failures and contributing to a culture of safety and improvement.
The activities EPAs focus on will vary according to the professional level a learner is being assessed on, and ranges with discipline and specialty. The flexible nature of EPAs means you need an equally flexible tool to assess learners in practice, such as MyProgress. The ability to author your own forms, add and edit them as needed gives each institution immense control.
The key question is: Can we trust this learner to carry out this EPA? The answer may be translated to levels of supervision for the EPA. The levels of supervision typically range from a learner needing close supervision right up to being ready for independent practice, on a scale that might look like this:
- Observation but no execution, even with direct supervision
- Execution with direct, proactive supervision
- Execution with reactive supervision
- Supervision at a distance and/or post hoc
- Supervision provided by the trainee to more junior colleagues
Irish College of General Practitioners
At MyKnowledgeMap we have lots of experience of working with EPAs within medical education. One example is with the Irish College of General Practitioners (ICGP). ICGP’s Training Programme is moving to competency based medical education, facilitated by EPAs. MyKnowledgeMap and the ICGP developed software (ICGP EPA) to capture feedback events and entrustment decisions from day-to-day clinical practice. Dashboard implementations bridge the gap between the large datasets and the training community at all levels.
Together we designed a MyProgress dashboard in which supervision levels are displayed in spider charts with each radius corresponding to an EPA, colour coded by level of supervision. Yellow/green denotes close supervision is required, and dark blue denotes distant supervision required. The summary view gives a wealth of information about a trainee in one glimpse, enabling medical educators to process larger datasets and helps with supervision level decision making. There is drill down functionality from the summary view to rich qualitative data of feedback comments.
Learn more about the project in this presentation.
As Karena Hanley, National Director for GP Training at the ICGP, puts it “The capacity to digest qualitative data allows a move away from tick box culture and focus on relevant data captured via regular low stakes feedback... promoting a holistic assessment in both definable dashboard implementations metrics and also in the undefinable ‘gut feeling’ of academic supervisors”
Western Sydney University
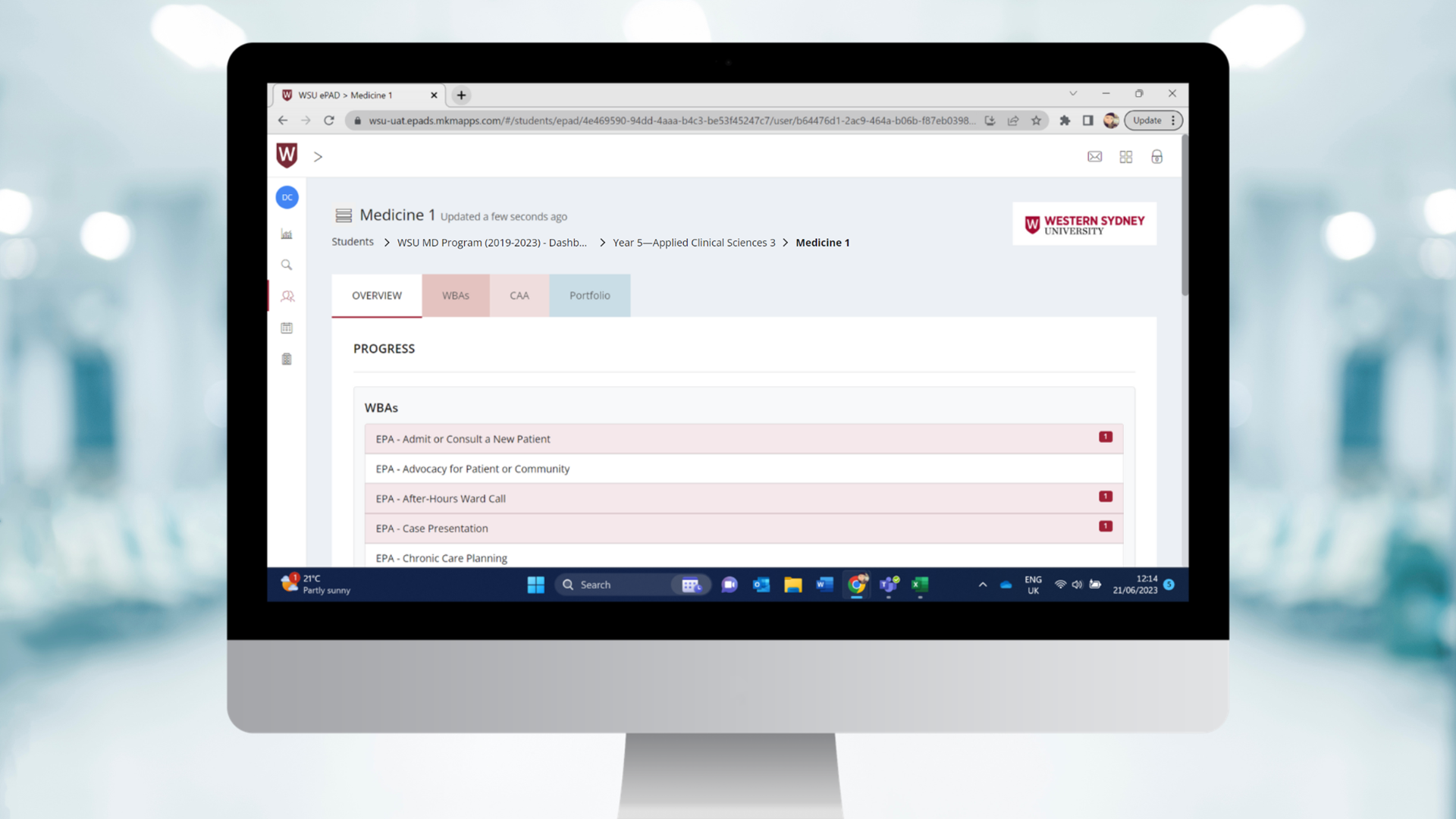
Another example of using MyProgress to measure EPAs in medical education is Western Sydney University. Western Sydney University use a customised MyProgress dashboard to visualise student progression using EPAs.

At a glance, educators can see real-time progress of a cohort of students, how many need close or distant supervision, and how many are safe to practice independently. They can also view individual student progress. They can zoom in on individual clinical schools, filter by dimensions such as case complexity, and see how students are performing against a cohort benchmark.
National EPA Frameworks for Clinical Curriculum Design
National organisations have developed frameworks for EPAs in undergraduate medical education. The Association of Faculties of Medicine of Canada (AFMC) and the Joint Commission of Swiss Medical Schools (SMIFK/CIMS) have published sets of EPAs that cover the full range of undergraduate medical education, including clinical rotations. These frameworks provide guidelines for the development and implementation of EPAs in various specialties and clinical settings.
The AFMC's framework includes twelve core EPAs, while the SMIFK/CIMS framework comprises nine core EPAs. Although there may be some differences in the number and wording of the EPAs across these frameworks, they all aim to define the essential competencies that medical students should possess by the end of their undergraduate education. These frameworks serve as valuable resources for medical schools and educators in designing curricula that align with competency-based education principles.
The Impact of EPAs on Medical Education and Healthcare
The introduction of EPAs in medical education has had a significant impact on the way competencies are defined, assessed, and integrated into curricula. By focusing on specific activities and responsibilities, EPAs help students develop the practical skills and knowledge necessary for independent practice.
Moreover, EPAs promote a culture of continuous improvement and patient safety. By identifying system failures and contributing to a culture of safety and improvement, students are equipped to become advocates for quality healthcare. The inclusion of EPAs in medical education curricula also enhances interprofessional collaboration, as students learn to work effectively as part of a healthcare team.
The implementation of EPAs is not without its challenges. Educators and institutions must invest time and resources in developing and validating EPAs specific to their curricula and clinical settings. Assessment methods must be carefully designed to ensure that students are evaluated accurately and fairly. However, the benefits of incorporating EPAs into medical education far outweigh the challenges, as they provide a more comprehensive and practical approach to training future healthcare professionals.
MyProgress: Empowering EPA Assessment and E-Portfolio Management
In the digital age of medical education, MyProgress has emerged to facilitate the assessment and monitor the progress of learners in undergraduate and postgraduate medical training. MyProgress is a powerful workplace-based assessment and e-portfolio tool that enables educators to measure and track students' progress in achieving EPAs. It provides a structured platform for documenting and assessing students' performance, allowing for comprehensive feedback and targeted support.
With MyProgress, educators can easily create assessment forms tailored to specific EPAs and track students' progress over time. The tool facilitates meaningful feedback and enhances the overall learning experience by promoting self-reflection, continuous improvement, and growth throughout a learner’s medical education journey.
MyProgress streamlines the assessment and management of EPAs, making the process more efficient and effective for both educators and students. It empowers learners to take control of their learning and assessment, and enables educators to provide personalised guidance and support, ultimately leading to the development of competent and confident healthcare professionals.
Explore MyProgress in the video below.
The Future of Medical Education: Progress in Competency
The integration of EPAs into medical education continues to build on competency-based training in practice. By shifting the focus from theoretical knowledge to practical skills and responsibilities, EPAs provide a more accurate and comprehensive assessment of students' readiness for independent practice. They bridge the gap between theory and practice, ensuring that learners are equipped with the competencies required for independent practice.
As medical education continues to evolve, the role of EPAs will become even more significant. The ongoing collaboration between medical schools, educators, and national organisations will shape the future of EPAs, refining their implementation and assessment. With tools like MyProgress, the measurement of EPAs and learner progress will become more streamlined and accessible, further enhancing the training of future healthcare professionals.
In conclusion, EPAs are transforming medical education by emphasising practical skills, teamwork, and a commitment to patient safety. As the landscape of healthcare evolves, competency-based training and the use of EPAs will continue to shape the future of medical education, ensuring that the next generation of healthcare professionals is prepared to meet the evolving needs of society. Assessing EPAs in medical education helps ensure that learners are prepared to provide safe and competent patient care as they progress through their training and into independent practice. With innovations like MyProgress, the assessment and management of EPAs become more efficient and effective, empowering educators and students alike. Together, we can revolutionise medical education and create a future where competence and expertise go hand in hand.
For more information about MyProgress or to learn how it would support your programme, please contact us by email at: myprogress@myknowledgemap.com
----------------------------------------------------------------------------------------------
References
https://onlinelibrary.wiley.com/doi/10.1111/j.1365-2929.2005.02341.x
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3613304/
https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-021-02608-9
Say Hello
Get in touch with the team
If you would like to discuss one of our learning technology platforms, or have an exciting project
you would like us to get involved in, feel free to get in touch with the team.
